Monkeypox: What is it? Q&A with infectious diseases specialist
Posted May 20, 2022 3:24 pm.
Last Updated May 20, 2022 5:48 pm.
The Public Health Agency of Canada confirmed two official cases of monkeypox in the country on Thursday night – both in Quebec. There were at least 17 suspected cases in and around Montreal, the city’s public health director had said earlier in the day. Also adding, there’s “no need to panic.”
We speak to infectious diseases specialist and medical microbiologist, Dr. Donald Vinh.
Can you break it down for us: What is monkeypox? How is it transmitted and spread?
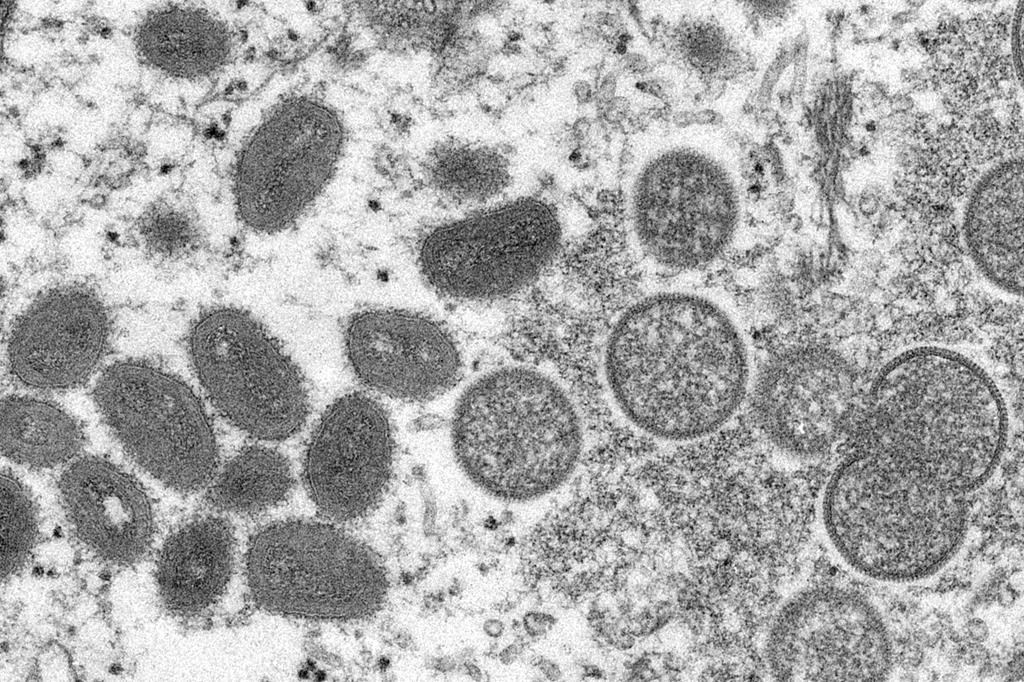
Monkeypox is caused by a virus that’s actually a cousin of smallpox. So, most of us won’t remember smallpox, but smallpox was a, you know, a pretty disfiguring virus that had a high death rate and was eradicated at the end of the seventies.
It’s cousin is what we’re talking about now. Monkeypox. Monkeypox is actually not from monkeys. It’s actually […] rodents and rats in Africa. And we know that over the last 40, 50 years, it’s caused outbreaks primarily in Africa and a little bit of sporadic cases in people who traveled to Africa and then went back to Europe or elsewhere.
The last outbreak we had in North America was actually in 2003. [Almost] 20 years ago. That’s a long time. So, it’s a very rare virus.
What it does is that when it infects people, it infects by one of two ways. You are either going to be in contact with an infected animal and then you’ll get either from their respiratory secretions or from that their bubbles on their skin, you’re going to get infected. […] You can get infected by either inhaling it or by a breaking of your skin where you get infected there.
When you get infected, what happens is that you get through two different phases. The first phase looks like you have the flu. You have a fever, you have a sore throat, you have a cough. That sounds like flu. Unfortunately, it also sounds like COVID. Both of them are actually circulating. So that’s going to be a bit of a problem to manage. Then after that, about a week after that episode, you’re going to start developing the pox.
When we say a pox, what that means is you get these skin lesions, you get these skin lesions that first start out flat, and then they become a bump, and then the bump becomes filled with fluid, and then it becomes white fluid and it happens all over your body.
But in monkeypox, it typically occurs on your hands and face, but also a little bit on the rest of your body. What’s what’s unusual in this cluster of cases is, first of all, there seems to be no relation to a travel to Africa, and there seems to be no relation to any known exposed or infected animals.
And all we’re seeing right now are clusters of cases, primarily among men, and they seem to be occurring in the genital areas primarily. So, for that unusual reason, there were about 17 or maybe even up to 20 suspected cases in and around the island of Montreal.
And as we heard last night, two are confirmed. And we are waiting to hear on more today.
How long does it take to recover? How is it treated and is it dangerous?
First of all, the illness can last somewhere around two to four weeks. And so you can imagine that you can actually be quite sick from it in terms of treatments. Unfortunately, there are no known treatments for monkeypox.
Where there monkeypox primarily is, which is in central and other parts of Africa, there aren’t the funds to do the research, and unfortunately there isn’t the interest to do any much research on it.
We don’t actually have any drugs available for monkeypox. So, when somebody gets sick with monkeypox and you can become quite sick – we know that from previous outbreaks, but you can become, you know, ICU sick.
We have to give supportive care. Now, there is a bit of a glimmer of hope, which is that in people who received the smallpox vaccine. So that was, you know, before, people were routinely getting the smallpox vaccine before 1970s, I think, in Canada.
And you do actually have some protection from monkeypox. Older studies have cited around 85 per cent. More recent studies suggest they may be lower because it has been so many decades between when people got the smallpox vaccine and when they were exposed to monkeypox.
What some public health authorities are doing in some countries, like in Europe, they’re actually going to try every time they have a confirmed case, they are going to try and do smallpox vaccination around the ring of people who are infected to try and mitigate the spread.
How should we be vigilant when it comes to this infection?
There was certainly no need for the public to panic, but there is certainly a strong need for the medical and scientific community to be on guard. And what does that mean on guard?
Well, that means that based on what we’re seeing, if there are people presenting to the clinics or to the hospitals with certain types of rashes that are unusual, perhaps also augmented by the fact that they may have been in contact with a known or suspected case or participate in some of the common activities that are related to that to these cases – there should be a protocol in place on how to isolate these patients and how to do the special tests to confirm that diagnosis. That’s what the medical and scientific community do.
Right now, we’re not dealing with a major outbreak that’s a threat to the public. It’s really confined to the people who are in direct contact with the confirmed cases.
So if you’re worried, well, can I get this from somebody who is at the grocery store as I’m going and get my loaf of bread and some milk? The answer is, look, low likelihood if you’re walking on the street or you’re going to go shopping in the grocery in the shopping malls, again, there’s a very low likelihood the cases that have been reported so far in Montreal seem to be related more to direct contact between the suspected or investigated cases and a confirmed case that’s traced back to Massachusetts.








